Chapter contents
Promoting Health and Wellbeing
Registering with GP, Dentist and Optician
Health Assessments and Health Plans
Strengths and Difficulties Questionnaire (SDQ)
Delegated Authority – Consent to Medical Treatment
Medication – Information, Rules and Guidance
Promoting Health and Wellbeing
The placing local authority has a duty to promote each fostered child’s physical, emotional and mental health. They have to act on early signs of health issues.
Children can come into foster care with health problems due to past neglect and missed health appointments. They need quick access to local health services to meet their needs. For this reason, every local authority has a Designated Doctor and specialist nurses who co-ordinate local provision for children in care. The nurses are often called LAC Nurses.
Every fostered child will have a health assessment and a health plan to identify and treat any health problems, and to promote general health and wellbeing. The LAC nurse might conduct the health assessment, and they are a good source of information and advice. The child’s social worker will give you their contact details if you need their help.
Foster parents should provide a healthy environment and help children and young people learn about healthy eating, physical activity, sex and relationships, smoking, alcohol and illegal substances. It is important that children learn to understand their own health needs, look after themselves and maintain a healthy lifestyle.
Complete the required training at Core grade: The health of a looked after child
For more information, see our Health and Wellbeing Policy
Read the Government’s guidance relating to the health of looked after children
Registering with a GP, Dentist and Optician
Unless the placement plan states that the child will remain with their current GP, you should register them with your GP straight away. A temporary registration is OK for very short-term placement, but most children will need a permanent registration so that their medical records transfer to the new GP practice. They will also be able to receive all the local health services they need.
You should also register the child with a local dentist and optician. The child’s social worker will be able to tell you when the child last saw a dentist or optician and when the next appointment is due. Often children in care have missed routine health appointments and may have unidentified needs that need addressing. Ensuring that they see key health professionals at regular intervals will inform the child’s Health Plan
Health Assessments and Health Plans
Every child who comes into care has an initial health assessment, carried out by a registered medical practitioner. This has to happen within 28 days of placement, which is when their care plan is first reviewed. The assessment is repeated every six months if the child is under 5, or every year for older children. The GP or LAC nurse can carry out these assessments, but children with complex health needs may have their health assessment with a paediatrician.
The Health Assessment will consider:
- The child’s current physical, emotional and mental health
- The child’s health history and family health history (where known)
- The effect of the child’s health on their development
- The child’s access to health services, including whether vaccinations are up to date.
Click here to see the current childhood vaccination schedule.
The health assessment informs the child’s health plan, which is part of their care plan. The health plan will identify key actions required to promote good health and wellbeing and address any health problems raised by the assessment. The plan will also clarify your role in responding to identified needs.
The child’s social worker should ensure that you receive a copy of the health plan. If you do not receive a copy, please notify your supervising social worker who will be able to request it on your behalf. If you receive a copy of the health plan through the post, please provide a photocopy to your local ISP Centre administrators, or your supervising social worker for our records.
Strengths and Difficulties Questionnaire (SDQ)
The SDQ is a reliable and valuable screening tool for mental health problems and can be used as evidence to support a referral to local mental health services. They are particularly helpful if completed just before the health assessment, to inform the health plan.
The child’s local authority will ask you to complete the SDQ as the main carer, and return it to them. Your supervising social worker will help you if needed. If you are able, please take a copy of the form before you send it back to the child’s social worker. We can upload this to the child’s CHARMS record at ISP.
Record Keeping
Each child’s CHARMS record at ISP includes health information. We will input known health problems and make a record of any medication or other treatment the child is receiving.
You are able to add some information to the child’s CHARMS record, eg:
- Please report when the child attends a health appointment. You can add these as ‘progress’ items, eg. “dentist appointment”.
- Please report when you give medication. You can add these as a ‘significant event’ (monitoring event – prescribed medication or monitoring even – non-prescribed medication).
- Please report injuries, accidents and illnesses. You can add these as a ‘significant event’ (monitoring event – injury, accident or illness, non-serious)
N.B. Report any serious illness or injury to ISP without delay. We will take care of the reporting.
You will discuss the child’s health with your supervising social worker at every supervision, and this is a good time to give them general updates.
Full instructions can be found in this guide. You will also receive training and support on CHARMS reporting from your local ISP centre.
Complete the mandatory training course: Recording & Reporting
Delegated Authority – Consent to Medical Treatment
The child’s placement plan will outline decisions that you are able to make as a foster parent. This is called ‘delegated authority’ and includes health and medication. The placement plan will state whether you can, for example:
- Give the child medication
- Sign a consent form for emergency and planned medical procedures
- Consent to the chid receiving routine vaccinations
- Consent to dental treatment
If the child needs medical treatment that you are not allowed to consent to then the doctor will contact the child’s local authority for consent. Hospitals have their own emergency procedures to ensure a child is treated without consent if necessary. Report all incidents to ISP as soon as possible.
If the child is over 16 they will usually be able to make their own medical decisions. A young person under 16 can request to make their own medical decisions and will be assessed for ‘Gillick competency’. This assessment is carried out by the health professional, e.g. the young person’s GP or a registered nurse at a young person’s sexual health service and considers their:
- maturity
- intelligence
- ability to make decisions and manage things like peer pressure, their family’s opinion and their own fears
- ability to consider the implications of their decisions
The child might be considered competent to make some decision but not others, depending on how serious the health problem is.
A young person who consents to their own medical treatment can request that certain aspects of their health be kept confidential between themselves and the health practitioner, and not shared with you or their social worker.
First Aid
Every fostering household should have a first aid kit for the treatment of minor injuries. Please keep an additional kit in each vehicle that children travel in.
The first aid kit should contain plasters and dressings to deal with minor injuries, for example:
- Alcohol-free cleansing wipes
- Plasters – a variety of sizes
- Micropore tape
- Crepe rolled bandages
- Burn dressings
- Gauze dressings (small, medium and large)
- Disposable gloves
- Safety pins
- Tweezers
The first aid kit should not contain any medication, and it does not need locking away. Store all medication securely, in line with the young person’s risk assessment.
Complete the mandatory training course: First Aid – book on ‘Learnative’.
Medication – Information, Rules and Guidance
- Always read the information leaflet for details of possible side effects
- If the young person is taking any prescribed medication, check with a pharmacist that it is safe to give them any over-the-counter medicines.
- Prescribed medication is only for the child whose name is on the label. Never give it to another child, even if they have similar symptoms.
- Check expiry dates, especially on over-the-counter medicines.
- Do not crush tablets or open capsules unless a doctor or pharmacist has indicated that it is safe to do so.
- Consult your GP if a child needs over-the-counter medicine for more than 48 hours.
- Do not give aspirin to young people under the age of 12 years unless it has been prescribed
- Give paracetamol or ibuprofen. Don’t give both at the same time, unless a doctor has advised you to.
- Do not give vitamin supplements or homeopathic remedies without consent from the child’s social worker.
- Keep a record of all medication given, on CHARMS (see ‘recording’ section above)
Managing problems
If a young person experiences side effects from medication, seek medical advice straight away. Do not discontinue the medication without instructions from the doctor or pharmacist, unless the child has had a severe reaction. Severe reactions include:
- difficulty breathing
- tingling sensation in the lips or mouth
- swelling to the lips, eyes, hand, face or body
- reddening of skin or blotching
In the event of a severe reaction, dial 999, reassure the child and keep them calm and notify ISP at the earliest opportunity, ensuring that the child is safe first.
In the event of a medication error (e.g. incorrect dose given, or incorrect medication given), contact the pharmacy and/or doctor and follow their instructions. Report the incident to ISP at the earliest opportunity, making sure that the child is safe first.
In an emergency, phone 999 and follow these general guidelines while waiting for help to arrive:
- Put the patient in the recovery position if possible. However, if they have fallen from a height, do not move them
- Try to find out what has happened in order to inform the emergency services
- Do not try to make the patient sick if they have swallowed something
- Observe the patient and keep them calm, warm and quiet
Report any serious accident or illness to ISP without delay. We will inform the Local Authority social worker and complete a significant event form.
Safe storage and disposal
Medication should be stored safety – out of reach of children and most likely in a locked cupboard. Your child’s risk assessment will confirm the expectations.
Always store medication in its original packaging. Some medication needs to be stored in the fridge and you may need a small locked box for this purpose.
Always dispose of medication when it reaches its use-by date. Medication should be returned to the pharmacy and never thrown in the bin, poured down the drain or flushed down the toilet.
Complete the mandatory training course: Medicines in the Foster Home – book on ‘Learnative’. An online alternative (Medication and Health Care) is available for secondary foster parents.
For more information, read our policy: Accidents, Illnesses, Medication & First Aid
Hospitalisation
Tell your supervising social worker, or the out-of-hours service, if a child is admitted to hospital. We will inform the child’s local authority and Ofsted.
Going into hospital is frightening and the child or young person is going to experience separation from people they know. In line with the principles of providing a secure base, you should, if possible, stay with and remain available to them in hospital. ISP may be able to provide assistance, if this means additional costs or the need for extra help.
Death of a Child
In the event of the death of a fostered child in your care, this is a summary of whom you should inform and what action you should take. The following procedures are designed to help at a time when everyone may be confused and distressed:
Who to notify
- Contact the relevant emergency services: doctor, ambulance, and police. Dependent upon the action they take, ensure that you know where the child is being taken.
- Immediately notify your supervising social worker, if possible by speaking to them personally. If they are not available, ask to speak to your registered manager, or another manager in ISP. Do not leave a message – insist on speaking to someone as a matter of urgency. If the death occurs out of normal hours you should immediately contact the ISP out-of-hours service.
- ISP will tell the child’s social worker, and children’s services will take responsibility for informing the child’s parents and anyone with parental responsibility.
- ISP is required to inform Ofsted and the Secretary of State of the death of a fostered child, within 24 hours. We/they may request further information, and it may be necessary to conduct a formal review of events before the child’s death. In the event of a sudden death there is likely to be an inquest, which you may be required to attend.
Funeral arrangements
- The child’s social worker will discuss with the parents the arrangements they wish to make about the funeral. Following the death of a child, any legal order on that child is no longer in place and the responsibility returns to the parents. This is a distressing time and sometimes parents and carers can disagree about funeral arrangements. It is the parents’ right to make decisions on these matters.
- Depending upon the parents’ wishes, you may be involved in the arrangements for the funeral.
- Your supervising social worker and registered manager will offer you and your family support and keep you informed of the procedures and the arrangements.
Healthy Eating
What is a healthy diet?
Children need regular meals and snacks to provide the energy and nutrients they need for growth and development. Meals should include items from the following food groups:
- Starchy carbohydrates such as potatoes, bread, pasta, rice, breakfast cereal (ideally wholegrain varieties)
- Fruit and vegetables (5 or more each day)
- Milk and dairy products such as yogurt and cheese
- Protein, such as meat, fish, eggs, beans, soya
Foods high in sugar should be avoided wherever possible and are best served with meals to protect dental health. Foods high in fat should be limited, although fat is an essential part of the diet, particularly aiding the absorption of vitamins A, D and E. Oily fish, milk, avocados and nuts are good sources of fat. Salt should not be added to children’s food and foods high in salt should be limited, e.g. potato crisps and ready meals.
Children should ideally drink water or milk to protect their teeth from decay. Fruit squashes and fizzy drinks are harmful to teeth and can contribute to excessive weight gain.
See https://www.bda.uk.com/food-health/food-facts.html for more information.
Developing healthy eating habits
Good healthy eating habits develop gradually and you will often be looking after children whose eating habits have developed in a deprived or unhappy atmosphere. Even where this is not the case, a child may refuse to eat unfamiliar food when they have just left home. All sorts of behaviours are possible; overeating, hoarding, stealing, being finicky, refusal, vomiting. Whatever the case may be, it is always best to avoid confrontation. Find out what the child’s eating habits and preferences are and only introduce new eating experiences gradually, at the child’s own pace. This is especially important for children with disabilities who may need special diets or help with eating.
Getting children involved in choosing and preparing their meals and snacks helps teach them about healthy eating and where food comes from, as well as developing an essential life skill. Visit the Eatwell Guide for more information.
Eating more fruit and vegetables
The Change4Life campaign gives the following advice for getting more fruit and vegetables into your diet:
- If you do not have time to prepare fresh vegetables try canned, frozen or pre packed and try stir-frying vegetables to improve flavour.
- Have fruit juice at breakfast.
- Keep a well-stocked fruit bowl.
- Snack on fruit or raw sticks of vegetable such as carrot, celery or peppers.
- Serve two types of vegetables with your dinner.
- Switch to fresh or dried fruit, breadsticks or unsalted nuts instead of sweets and biscuits.
Dietary supplements (e.g. vitamins)
If a child has been malnourished or has a restricted diet, and you are concerned that they may not be gaining the required amounts of vitamins and minerals from food each day, please speak with their social worker and GP about the possible benefits of vitamin supplements. As with all medications, please do not give vitamin supplements without the permission of the child’s social worker and without medical advice.
If the child’s Health Plan indicates the need for a vitamin supplement, please ensure that this is provided.
Physical Activity
All young people need at least one hour’s exercise each day. Regular exercise strengthens muscles and bone and contributes to good cardiovascular health. It also helps children maintain a healthy weight.
Sporting clubs, e.g. football, gymnastics and karate help children to keep active while making friends and achieving new skills. In addition to these regular activities, try and increase activity each day by:
- Walking or cycling rather than going by car
- Taking the stairs rather than the lift
- Walking a dog
- Going to the local park
- Family bike rides
- Encouraging outdoor play
The Change4life website has lots of ideas for everyday family activities that can help children do 60 minutes of physical activity every day.
Change4life – https://www.nhs.uk/change4life/activities
Explore a range of leisure activities in your area, sporting or not, and encourage young people to try those that interest them. Many children will need a lot of help and encouragement to find interests they enjoy and there may be ‘false starts’ along the way. It is normal for children to try out several activities before they find one that really suits them, and it is important to be patient with them.
Children’s activities can become very expensive over time, if they develop a strong talent for something. If the costs are more than you consider reasonable, talk to your supervising social worker as you might be able to get some help with this. For example, the Spark Foundation awards small grants for children in care and care leavers, and you could apply for help to buy an expensive piece of equipment.
Sex and Relationships
Talking about relationships and sex
Sex should be seen as a normal and healthy part of adult relationships. It is important that children are able to learn and talk about healthy relationships, and their own sexual development, within the family home. They need to be prepared for the changes that will take place in their bodies, and helped to understand their feelings and emotions during puberty. Older young people will also need information about the law and consent – including an understanding of sexual assault and rape.
Age-appropriate conversations should take place at home, particularly if the child asks a question. Children will be receiving information from lots of places – not all of it true – and simple answers to their questions can help them to understand. A child who understands is a confident child.
Sometimes conversations are difficult because different families, cultures and religions have their own sets of values about sex and relationships. You might be caring for a child whose attitudes are different to yours, or you might be looking after a child who has experienced abuse and exploitation in the past. An open and sensitive approach will help young people to learn that they can come to you with their questions and for help if they need it.
Sexual orientation and gender identity
Happiness comes from being accepted for who we are – not living life according to the wishes of those who care about us. If a young person feels that they are lesbian or gay, transgender or non-binary (or they are unsure), then talking to somebody who understands will help. Ideally, that person will be you, but it could also be another family member, a friend, their social worker or perhaps a counsellor.
Everyone needs the support, acceptance and understanding of those who are caring for them. Lots of people make different choices about their partners, often in the face of prejudice and hostility from those around them. Your supervising social worker and the child’s social worker will be able to advise and put you in contact with additional support services, groups or help lines that the young person can contact for advice.
If a young person is experiencing distress regarding their biological sex and gender identity (known clinically as gender dysphoria), you should consult with their GP about a referral to your local CAMHS service. Services for children and young people are currently under review by the NHS and you can read more information about this here:
Sexual Health and Contraception
Young people, including those under 16, need reliable information on sexual health and contraception. They also need to know where they can get advice and treatment. Let your young people know that they can receive a free and confidential service from:
- Their own GP
- A local sexual health service (these often have young people’s clinics)
- Brook Advisory Centres (where available)
Health professionals can give contraceptive advice and treatment to young people under 16 without their parents’ consent, if they consider the young person to be ‘Gillick competent’. Young people under care orders have the same right to confidentiality and treatment from health professionals as other young people.
Foster parents cannot give consent for a young person to receive contraception and this should be referred to the child’s social worker if the young person has not been judged competent to make their own sexual health choices.
For more information, read our Sexual Health: Consent & Confidentiality policy:
Training opportunity: Promoting Sexual Health
Pregnancy
Some young people have a strong desire for a baby, particularly if their own childhood was unhappy. Research with teenagers who planned a pregnancy showed that they were often looking to create a family of their own, with love and stability that they may not have experienced in their own early years. Motherhood also offered an identity for some young girls who did not have a good self-esteem or clear career pathway.
Whether planned or unplanned, pregnancy needs to be dealt with sensitively. Together with the child’s social worker and your supervising social worker, you should help the young woman through her pregnancy and support whatever decision she makes about her baby. She may need help to decide whether to keep her baby, ask her family for support, or consider adoption, but it is her decision to make. If a young man is about to father a child, he will have feelings too. He must know that he can talk to you. He may also need professional advice on such matters as ‘parental responsibility’.
Sexually transmitted infections (STIs)
Encourage and support your young people to learn about STIs and protect themselves if they are sexually active. Let them know where they can get factual information, and where they can go for advice and treatment. Young people can get information and advice about STIs from:
- Their own GP
- A local sexual health service (these often have young people’s clinics)
- Brook Advisory Centres (where available)
- The Sexwise website
If you know, or suspect that a young person has an STI (including HIV), please let your supervising social worker know. They will contact the young person’s social worker and together you will help the young person get the treatment they need.
Alcohol
Alcohol is often associated with pleasure, relaxation and socialisation. However, it is a drug that can harm both physical and mental health. Some fostered young people have lived with adults who misuse alcohol, and this will have shaped their own attitudes towards alcohol. Others will have cultural or religious beliefs that forbid the use of alcohol. It is important that young people can talk with you about how they feel.
Young people often try alcohol for the first time as teenagers, and this is often in the company of friends. At this age, they might not recognise the potential risks:
- Accidents – alcohol affects balance, co-ordination and risk perception
- Violence and aggression – alcohol affects emotions and behaviour, and some people become aggressive
- Unprotected sex – when we drink alcohol we lose our inhibitions and can act impulsively. This can lead to unplanned pregnancy and STIs
- Alcohol poisoning – drinking large amounts of alcohol can lead to loss of consciousness and death.
Please talk with your young people about alcohol and healthy lifestyle choices. Always model sensible use of alcohol in the home.
The law and alcohol
Young people under 18 can be stopped, fined or arrested if they are caught drinking alcohol in public. It is illegal for them to buy or try to buy alcohol, and it is illegal for shops to sell them alcohol.
The law permits parents to allow their children, over the age of 5 years, to drink alcohol in the home. A young person over 16 is also allowed to drink (but not buy) alcohol in a pub or restaurant as part of a meal with their parents.
Foster parents cannot, without the permission of the Local Authority and anyone else with parental responsibility, give alcohol to a young person in foster care. Where permission has been given, the Chief Medical Officer for England’s guidance should be followed. This guidance states that:
- An alcohol free childhood is the healthiest option. However, if children drink it should not be until, at least, the age of 15 years.
- If young people aged 15 to 17 years consume alcohol it should always be with the guidance of a carer or in a supervised environment.
- Foster parents and young people should be aware that drinking even at the age of 15 or older can be hazardous to health. If 15 to 17 year-olds do consume alcohol they should do so infrequently and certainly on no more than one day a week.
- Young people should never exceed the recommended adult daily limits when they drink. Consumption should usually be below such levels. (The maximum recommended intake in one day is 2-3 units for women and 3-4 units for men)
Read the Chief Medical Officer’s guidance here:
For more information, see our Alcohol, Drugs and Solvents policy:
Training opportunity: Smoking, Alcohol and Drugs
Smoking
Smoke free environments
“Smokefree” law, introduced in 2007, banned smoking in both the work place and indoor areas which are used by the public. All ISP premises are subject to this legislation which applies to both staff and visitors. The law was extended in October 2015 to include a ban on smoking in cars with a child under the age of 18 years present.
Smoking, and exposure to second-hand smoke (“passive smoking”) is harmful to health both in the short and long-term – with harm to the lungs and heart in particular. Children exposed to cigarette smoke are at risk of developing lung diseases, including asthma, and exposure can make existing conditions worse. We expect all of our foster homes to be smoke-free environments. In addition, nobody should smoke in a vehicle with a child.
ISP will not make the following placements with any foster family who has a smoker living in the household:
- Children under the age of 5 years.
- Parent and child.
- Child of any age with a respiratory illness which is known to be aggravated by smoke.
Where foster parents do smoke, the issue will be discussed at supervision and annual review. ISP will always encourage our foster parents to give up smoking and provide support throughout the process.
Young people and smoking
While research shows that smoking among young people is in decline, many young people continue to try smoking, and some of these will become regular smokers. Some young people in foster care smoke and you should encourage and support them to reduce and ultimately give up smoking. Young people can get support to give up from their GP. The NHS “smokefree” website is also a helpful resource.
It is against the law to buy cigarettes for young people under the age of 18 years – if you are looking after young people who smoke you must not buy cigarettes for them. Smoking should be discussed with the young person’s social worker and a plan for managing this included within the health plan and the risk assessment.
ISP will respect your wishes if you choose not to foster young people who are known to smoke and you should inform the placements team if you do not wish to be considered for such placements. Young people who do smoke must not be permitted to smoke within your home, and you should inform the young person of the house rules on smoking before, or at the start of placement.
Electronic Cigarettes
The same rules apply to electronic cigarettes (‘vapes’) as to smoking. The potential health risks of vaping is currently unknown and their sale is restricted to over-18s.
Information about smoking and its effects on health is available from ASH.
For more information, read our Smoking Policy.
Training opportunity: Smoking, Alcohol and Drugs
Illegal Drugs
What are illegal drugs?
‘Illegal’ drugs are substances which are controlled under the Drugs Act (2005) and the Misuse of Drugs Act (1971). The law places illegal drugs into three different categories, or ‘classes’. These classes (A, B and C) carry different penalties for possession and dealing. The following Home Office website provides information about the classification of drugs and maximum penalties: http://www.homeoffice.gov.uk/drugs/drug-law/
Some examples
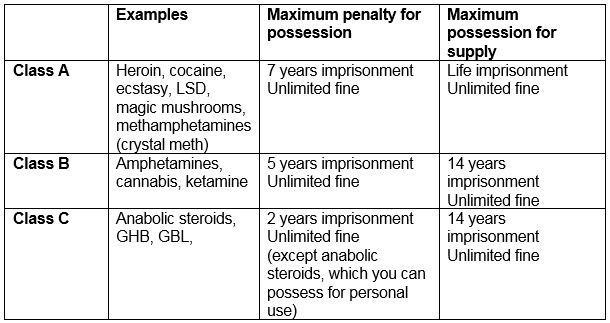
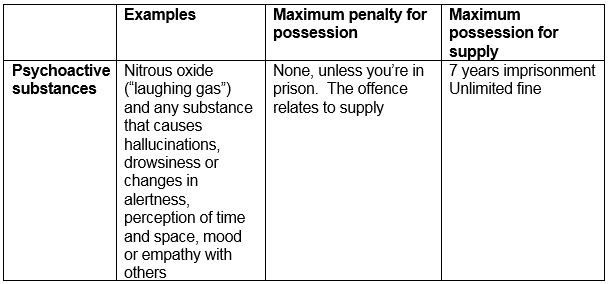
The Psychoactive Substances Act (2015) addressed the problem of ‘legal highs’ by outlawing any substances that have a psychoactive effect, when they are sold for this purpose.
Talking with young people about drugs
You need to be able to talk with young people about drugs and help them make healthy lifestyle choices. Some young people in care will have experienced living in households where drugs were abused, and some will have been exposed to drugs in the womb. Other young people will have cultural or religious beliefs that forbid drug use. It is important that young people can talk with you about how they feel about drugs and ask questions as they arise.
Some young people will come into contact with drugs as they get older, often in the company of friends. At this age many young people will not appreciate the potential dangers of drugs, or be aware of what they are taking, or their effects. They are likely to receive mixed messages from peers, adults and the media. Young people who are upset and troubled are especially vulnerable to using substances that offer a change of mood or consciousness.
Young people in care may get involved for many reasons. These can be to escape from painful experiences, to seek attention, to rebel, to take risks, or to bow to the pressure of their friends and acquaintances. Whatever the reason they have used drugs, it is important to try to talk openly with them to help them make informed and healthy lifestyle choices.
Our Tips:
- Remind young people of your views and the house rules, but also let them know that they can come and talk to you if they have a problem or are worried.
- Use opportunities to give young people knowledge about drug use along with the support services that are around.
- Ask them what they are learning at school about alcohol, smoking and drugs.
- Reinforce their sense of self-worth through demonstrating your acceptance of who they are. This will assist them to be able to make good decisions and keep themselves safe.
- Encourage them to develop positive values around their own health choices and explore with them how to resist peer pressure.
Common symptoms of drug misuse
There are many warning signs of drug use and abuse. The challenge for foster carers is to distinguish between the normal, sometimes volatile, ups and downs of puberty and the teenage years, and the red flags of drug abuse.
Physical warning signs of drug abuse
- Bloodshot eyes or pupils that are larger or smaller than usual, or use of eye drops to mask this.
- Changes in appetite or sleep patterns. Sudden weight loss or weight gain.
- Deterioration of physical appearance and personal grooming habits.
- Unusual smells on breath, body, or clothing.
- Tremors, slurred speech, or impaired coordination.
- Using incense, perfume, or air freshener to hide the smell of smoke or drugs.
Behavioural warning signs of drug abuse
- Drop in attendance and performance at school or work.
- Unexplained need for money or financial problems.
- Missing money or personal possessions
- Being secretive about friends, possessions, and activities.
- Sudden change in friends, favourite hangouts, and hobbies.
- New interest in clothing, music, and other items that highlight drug use.
- Frequently getting into trouble (fights, accidents, illegal activities).
Psychological warning signs of drug abuse
- Unexplained change in personality or attitude.
- Sudden mood swings, irritability, or angry outbursts.
- Periods of unusual hyperactivity, agitation, or giddiness.
- Being unusually isolated, withdrawn, or depressed.
- Demanding more privacy – locking doors, avoiding eye contact, sneaking around.
- Lack of motivation – seems very tired or “spaced out.”
- Seems fearful, anxious, or paranoid, with no reason.
If you find out that a young person is, or has been using drugs, you need to report this to ISP and discuss with your supervising social worker and the young person’s social worker how best to manage the situation. Some young people might need specialist help to deal with a drug habit and ISP will be able to help make a referral to these services.
Visit the FRANK website for further information about drugs.
What if I find drugs in my home?
If you find any substances in your home which might be illegal drugs, report this immediately to your supervising social worker, manager, or ISP out-of-hours service. They will inform the young person’s social worker.
All drugs and unidentified substances must be passed to the police for safe destruction, although our procedures are designed to avoid the unnecessary criminalisation of young people. Please read our guidance here:
Training opportunities: Smoking, Alcohol and Drugs, and Introduction to Drug Awareness (for a more detailed coverage)
For more information, see our Alcohol, Drugs and Solvents policy:
Infectious Diseases
Infectious diseases are caused by organisms such as bacteria, viruses, fungi and parasites. Some infectious diseases are passed from person to person – these are called contagious diseases. Many infectious diseases can be controlled through routine vaccination in childhood (e.g. Measles, Rubella) and a fostered child’s first health assessment will look at their vaccination history.
You can see the current UK vaccination schedule here.
Advice on managing infectious diseases, including school exclusion times can be viewed here.
Some contagious diseases are passed from person to person through bodily fluids or pregnancy, and some children will have been infected in this way as a result of a parent being infected. This includes a risk of HIV and Hepatitis B. A young person might be tested if there are concerns about infection.
HIV and AIDS
HIV (Human Immunodeficiency Virus) is a virus which damages the body’s immune system and weakens its ability to fight infections and disease. There is no cure for HIV, but there are treatments which help most people with the virus to live a long and healthy life. AIDS is the final stage of HIV infection, when the immune system has lost the ability to fight illness. Most people with HIV infection today will not go on to develop AIDS.
HIV is transmitted through blood, semen, vaginal and anal fluids, and breast milk. Transmission is therefore possible through unprotected sex, pregnancy and childbirth, breastfeeding and using contaminated needles and syringes. HIV is not transmitted through sweat or urine nor normal contact and activities, e.g. coughing, sneezing, kissing, hugging or sharing bathrooms.
Further information about HIV in childhood can be found at the Chiva website.
Hepatitis B and Hepatitis C
Hepatitis is a term used to refer to inflammation of the liver. There are several different types of hepatitis virus – you can read about them all on the NHS website.
Hepatitis B and Hepatitis C are both contagious and passed from person to person through blood, semen and other bodily fluid. Children may become infected during childbirth if their mother is infected. Hepatitis is not spread by normal daily contact, coughing, sneezing, kissing, hugging, holding hands or sharing a bathroom.
Children with Hepatitis B and C often have no symptoms. Symptoms that can occur include fatigue, aches and pains, jaundice (yellowing of the skin and eyes and dark urine), nausea, vomiting, itching and loss of appetite. Long-term infection can cause liver damage which is more severe with Hepatitis B. For this reason, infected children will need specialist treatment.
Confidentiality
A child’s HIV/Hepatitis status is confidential and should only be disclosed on a need-to-know basis, in the interests of the child.
The child and those with parental responsibility should always consent to disclosure.
Infection control
The following hygiene and infection-control procedures should be used in all homes. We may be aware of some infections and not others, and these procedures can help reduce the risk of any infection begin transferred.
- Do not share towels, face cloths, razors or toothbrushes.
- Cover minor cuts with a waterproof plaster.
- Wrap sanitary products and nappies before placing in a bin.
- Clean kitchen and bathroom surfaces with a general household cleaner. Either use a disposable cloth or wash cloths after every use in hot, soapy water and leave to dry fully.
- Surfaces soiled by body fluids should be cleaned immediately with bleach or disinfectant.
- Crockery and cutlery can be shared. Wash after every use with hot soapy water or in a dishwasher.
- Use disposable gloves if cleaning up body fluids, and cover any cuts or wounds on your hands with a waterproof dressing.
- Wash your hands immediately if they come into contact with body fluids.
Young people with HIV or Hepatitis infection should be informed about the importance of using condoms and never sharing needles if they are using drugs.
Mental Health
What is mental health?
Mental health concerns both our general psychological wellbeing, and mental health problems.
Psychological wellbeing:
Our psychological wellbeing includes our self-esteem, feelings of control, sense of belonging and purpose, and satisfaction with life. It helps us to cope with life and play an active part in relationships and work. With good mental health we can achieve our potential.
Psychological wellbeing doesn’t mean feeling happy all the time. Our feelings are affected by situations and it is natural to feel sad or angry if something bad happens. It is equally natural to feel anxious when things are going wrong. Part of developing good mental health and wellbeing in children and young people is helping them recognise that it is natural to feel different emotions. The important thing is that they can ask for help when they need it, and they know who can help them.
Mental health problems:
Mental health problems are diagnosable conditions that significantly interfere with our feelings and thought processes. They can affect our ability to cope with life and do the things that we need to do.
Some of these conditions are called ‘neuroses’ and these include depression and anxiety. They are considered to be extreme forms of normal emotional experiences, and are quite common.
Other conditions are known as ‘psychoses’ and these are less common. They involve altered states of reality, such as hallucinations (e.g. seeing and hearing things that no-one else can).
Mental health problems in childhood include:
- Eating disorders
- Attachment disorders
- Generalised anxiety
- Obsessive-compulsive disorders
- Depression
- Attention Deficit Hyperactivity Disorder (ADHD)
What can foster parents do to promote good mental health and emotional wellbeing?
The most important thing that all carers can do is to offer a secure base environment to children and young people (see chapter 9). A secure base helps children to trust the adults who care for and are available to them. It also develops positive self-esteem and helps children develop some of the social, emotional and behavioural skills that promote good mental health. These include:
- Build and sustain friendships.
- Deal with and resolve conflicts.
- Solve problems both with others and alone.
- Manage strong feelings such as frustration, anger and anxiety.
- Recover from setbacks.
- Work and play co-operatively.
- Compete fairly and lose with dignity.
- Respect the rights of others.
Practical things you can do at home:
- Encourage children and young people to join local clubs so they get a sense of achievement from doing something they enjoy as well as forming new friendships.
- Celebrate achievements at school and support school work.
- Encourage children to express themselves, make choices and talk about how they feel.
- Do things together that enhance a sense of achievement such as cook a meal, bake a cake, go on bike ride, learn a new computer game.
- Do not overprotect children by avoiding challenging situations that may help them problem solve or develop emotional skills such as negotiating new friendships.
Young Minds website
Take the time to look at the Young Minds website and raise your own awareness about what young people themselves say helps them.
Here is a leaflet by Young Minds about self-harm. This leaflet is written for both young people and their families.
University of Oxford researchers have also released a helpful leaflet for parents and carers about self-harm.
Training opportunities: Mental Health Awareness, plus additional courses covering eating disorders, anxiety, psychosis, self harm, depression, suicide, addiction within the family, and drug awareness. Book on ‘Learnative’.
ISP Therapeutic Model
Our young people have often had a painful history that has deeply affected their development. We believe that these children need therapeutic care to reach their emotional, social and educational potential.
Our young people have experienced things as having gone very wrong in their lives and are likely to have been traumatised by this. This often results in behaviour that adults find difficult to manage at home and at school. We see our task as that of providing an integrated service connecting with the child or young person who is likely to be in a state of panic and distress. We aim to contain, understand, empathise and best manage their behaviour as we gradually help them to feel safe and able to develop within long term meaningful relationships.
The most crucial relationship for the child is with their foster family. Everyday caring experiences can be therapeutic, especially for children who have not received good enough parenting during their early years. We believe that our foster parents are in a strong position to meet the children’s emotional needs, but that you need our support to work through the challenges and difficulties that arise. As well as offering therapy to our children and young people, our therapy service also offers support to our foster parents.
Our therapy team includes psychotherapists, speech and language therapists and counsellors. We can also access support from psychiatrists and educational psychology services.
We can offer…
- Assessment and consultation regarding a child’s needs, and to support placement stability.
- Assessment of emotional, behavioural and therapeutic needs in preparation for permanence.
- Time-limited direct therapy with young people and/or their foster parents regarding mental health needs.
- Therapeutic parenting groups for foster parents.
- A range of ‘Reflective Practice’ groups for foster parents and staff.
CAMHS
Most of our young people receive their therapy support from our therapists. Some, however, will receive a service from CAMHS (Child and Adolescent Mental Health Service). This is an NHS service that provides mental health assessment and treatment for children and young people. The service targets children with diagnosed or suspected mental health problems.
CAMHS teams include occupational therapists, child and family counsellors, specialist nurses, clinical psychologists, psychiatrists, social workers, family support workers and psychotherapists. Most local CAMHS services have waiting lists and it can be several months before a child is seen. If you think a child or young person would benefit from the CAMHS service, talk with your supervising social worker and the child’s social worker about your concerns straight away.



